
As part of our women’s health series, we are highlighting common reasons women in their 30s visit the gynecologist.
We spoke with Dr. Prethi Vaddadi, of SIMED Women’s Health, about why women go to the gynecologist, how their common problems are treated and what to look for in common gynecological issues.
Vaginitis:
Vaginitis is an inflammation of the vagina. As many as one third of all women will experience symptoms of vaginitis during their lives. Vaginitis is most common during the reproductive years.
A change in the balance of the yeast and bacteria that normally live in the vagina or a shift in a woman’s hormone levels can result in vaginitis. Symptoms associated with vaginitis include: change in color, odor or amount of vaginal discharge, itching or irritation, pain during intercourse, spotting or light vaginal bleeding, and/or painful urination.
Factors that can change the normal balance of the vagina include:
1. Use of antibiotics
2. Changes in hormone levels due to pregnancy, breastfeeding, or menopause
3. Douching,
4. Spermicides
5. Sexual intercourse
6. Infection.
To diagnose vaginitis, your health care provider will take a detailed history, examine the area and take a swab of the discharge from your vagina.
Common causes of vaginitis:
1. Yeast infection (candidiasis)
Yeast infection is a common cause of vaginitis. The yeast infection is usually caused by a fungus called Candida. It is found in small numbers in the normal vagina. However, when the balance of bacteria and yeast in the vagina is altered, the yeast may overgrow and cause symptoms.
Symptoms may include:
1. Itching and burning of the area outside the vagina called the vulva
2. Red and swollen vagina
3. White, lumpy, odorless vaginal discharge
Yeast infections can be treated either by placing anti-fungal medication into the vagina or by taking a pill.
2. Bacterial Vaginosis:
Bacterial vaginosis is caused by a shift in the quantity of a particular bacteria normally occurring in the vagina.
Symptoms:
The discharge is usually thin and dark or dull gray, but may have a greenish color. Itching is uncommon, but may be present if there is a lot of discharge. The discharge odor is described as fishy, but may only be noticeable after sexual intercourse.
Treatment:
Several different antibiotics can be used to treat bacterial vaginosis, but the two that are most commonly used are metronidazole and clindamycin. They can be prescribed to be taken by mouth or via insertion into the vagina as a cream or gel.
3. Atrophic Vaginitis:
This condition is not caused by an infection, but may occur any time when female hormone levels are low, such as during breastfeeding and after menopause.
Symptoms:
Atrophic vaginitis results in vaginal irritation, such as dryness, itching, burning, changes in urination, change in vaginal discharge, and/or painful vaginal intercourse.
Treatment:
Atrophic vaginitis is treated with estrogen, which can be applied as a vaginal cream, ring, or tablet. A water-soluble lubricant also may be helpful during intercourse.
Sexually Transmitted Infections:
A person with an STI (Sexually transmitted infection) can pass it to others by contact with skin, genitals, mouth, rectum, or body fluids. Anyone who has sexual contact—vaginal, anal, or oral sex—with another person may get an STI. STIs may not cause symptoms. Even if there are no symptoms, your health can be affected.
STIs are caused by bacterial or viral infections. STIs caused by bacteria are treated with antibiotics. Those caused by viruses cannot be cured, but symptoms can be treated.
Common STIs: Chlamydia, Gonorrhea, Genital Herpes, HIV, HPV, Syphilis, Trichomoniasis, Hepatitis B
How can you reduce the risk of getting an STI?
Know your sexual partners and limit their numbers. The more partners you have or your partners have had, the higher your risk of getting an STI.
Using a latex condom every time you have vaginal, oral, or anal sex decreases the chances of infection. Condoms lubricated with spermicides do not offer protection against STIs, and in fact, frequent use of some spermicides can increase the risk of HIV.
Sexual acts that tear or break the skin carry a higher risk of STIs. Even small cuts that do not bleed let germs pass back and forth. Anal sex poses a high risk because tissue in the rectum tears easily. Body fluids also can carry STIs. Having any unprotected sexual contact with an infected person poses a high risk of getting an STI.
Vaccines are available to greatly reduce the risk of Hepatitis B and HPV infections and should be received by anyone at moderate to high risk.
Contraception: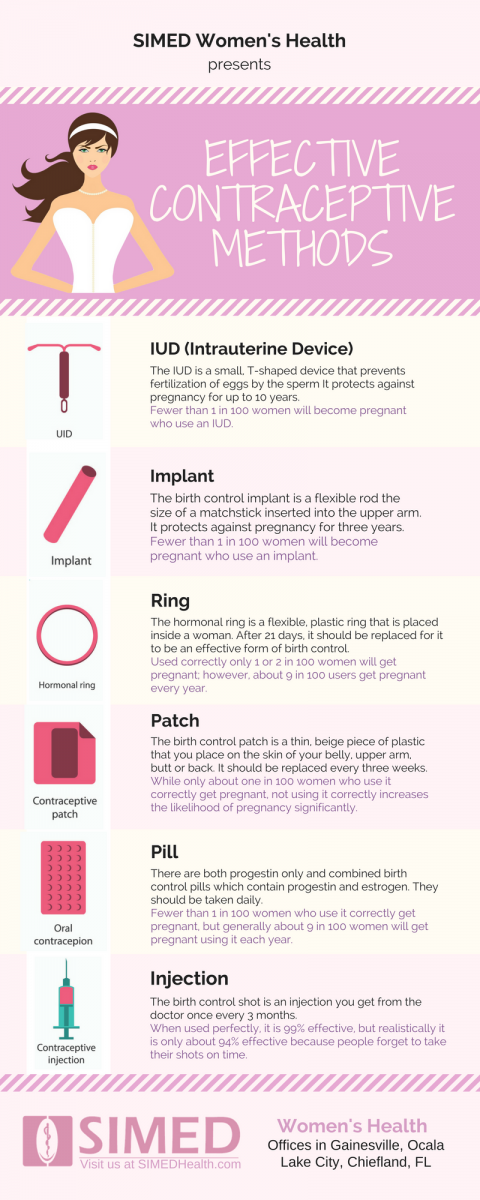
1. Long Acting Contraceptives
Long-acting reversible contraception (LARC) methods include the intrauterine device (IUD) and the birth control implant. Both methods are highly effective in preventing pregnancy, last for several years, and are easy to use. Both are reversible—if you want to become pregnant or if you want to stop using them, you can have them removed at any time.
The IUD and the implant are the most effective forms of reversible birth control available. During the first year of typical use, fewer than 1 in 100 women using an IUD or an implant will become pregnant. This rate is in the same range as that for sterilization.
Over the long term, LARC methods are 20 times more effective than birth control pills, the patch, or the ring.
IUD:
The IUD is a small, T-shaped, plastic device that is inserted into and left inside the uterus. There are two types of IUDs:
1. The hormonal IUD releases progestin. Different brands of hormonal IUDs are approved for use for up to 5 years and for up to 3 years.
2. The copper IUD does not contain hormones. It is approved for use for up to 10 years.
Both types of IUDs work mainly by preventing fertilization of the egg by the sperm. The hormonal IUDs also thicken cervical mucus, which makes it harder for sperm to enter the uterus and fertilize the egg, and keep the lining of the uterus thin, which makes it less likely that a fertilized egg will attach to it.
Implant:
The birth control implant is a single flexible rod about the size of a matchstick that is inserted under the skin in the upper arm. It releases progestin into the body. It protects against pregnancy for up to 3 years.
The progestin in the implant prevents pregnancy mainly by stopping ovulation. In addition, the progestin in the implant thickens cervical mucus, which makes it harder for sperm to enter the uterus and fertilize the egg. Progestin also keeps the lining of the uterus thin, making it less likely that a fertilized egg will attach to it.
2. Combined Birth Control Methods:
Birth control pills, the birth control patch, and the vaginal birth control ring are combined hormonal birth control methods. They contain two hormones: estrogen and progestin.
These hormones prevent pregnancy mainly by stopping ovulation (the release of an egg from one of the ovaries). They also cause other changes in the body that help prevent pregnancy. The mucus in the cervix thickens, making it hard for sperm to enter the uterus. The lining of the uterus thins, making it less likely that a fertilized egg can attach to it.
With perfect use—meaning that the method is used consistently and correctly each time—fewer than 1 woman out of 100 will become pregnant during the first year, according to the American Congress of Obstetricians and Gynecologists.
Vaginal Ring:
The vaginal ring is a flexible, plastic ring that is placed in the upper vagina. It releases estrogen and progestin that are absorbed through the vaginal tissues into the body.
You fold the ring and insert it into the vagina. It stays there for 21 days. You then remove it and wait 7 days before inserting a new ring. During the week the ring is not used, you will have your period.
3. Progestin only contraception methods:
Progestin is a form of progesterone, a hormone that plays a role in the menstrual cycle and pregnancy. Progestin-only pills and the injection have about the same effectiveness as combination estrogen and progestin pills, rings, and patches.
Abnormal Uterine Bleeding:
The normal length of the menstrual cycle is typically between 24 days and 38 days. The vaginal bleeding in a cycle is usually 4 to 6 days, but can last up to 8 days.
Bleeding in any of the following situations is considered abnormal uterine bleeding:
1. Bleeding or spotting between periods
2. Bleeding or spotting after sex
3. Heavy bleeding during your period
4. Menstrual cycles that are longer than 38 days or shorter than 24 days
5. “Irregular” periods in which cycle length varies by more than 7–9 days
6. Bleeding after menopause.
Some of the causes of abnormal bleeding include:
1. Problems with ovulation
2. Fibroids and polyps
3. Adenomyosis, a condition in which the endometrium (or inner lining of the uterus) grows into the wall of the uterus
4. Bleeding disorders
5. Problems linked to some birth control methods, such as an intrauterine device (IUD) or birth control pills
6. Miscarriage
7. Ectopic pregnancy (fertilized egg implants outside the uterus)
8. Certain types of cancer, such as cancer of the uterus and cervix.
Abnormal uterine bleeding is diagnosed by obtaining a detailed health history of you and your menstrual cycle. It may be helpful to keep track of your menstrual cycle before your visit. Note the dates, length, and type (light, medium, heavy, or spotting) of your bleeding on a calendar. You also can use a smartphone app designed to track menstrual cycles. Blood tests may be done to rule out other diseases.
Treatment of Abnormal Uterine Bleeding:
Medications often are tried first to treat irregular or heavy menstrual bleeding.
If medication does not reduce your bleeding, a surgical procedure may be needed. There are different types of surgery depending on your condition, your age, and whether you want to have more children.
Abnormal Cervical Screening (Pap Smears):
Cervical cancer screening is used to find abnormal changes in the cells of the cervix that could lead to cancer. The cervix is the portion of your uterus that extends down into the vagina. Screening includes the Pap test and, for some women, testing for a virus called HPV.
The main cause of cervical cancer is infection with HPV. If you have an abnormal cervical cancer screening test result, you may need further testing.
Treatment:
In general, there are two ways to treat abnormal cervical cells: 1) “excisional” treatment and 2) “ablative” treatment. With excisional treatments, tissue is removed from the cervix and is sent to a laboratory to be studied. The results will determine the severity of abnormal cells. With ablative treatment, abnormal cervical tissue is destroyed, and there is no tissue to send to a laboratory for study.
Polycystic Ovary Syndrome (PCOS):
Common PCOS signs and symptoms include the following:
• Irregular menstrual periods
• Infertility
• Obesity
• Excess hair growth on the face, chest, abdomen, or upper thighs
• Severe acne or acne that occurs after adolescence and does not respond to usual treatments
• Oily skin
• Patches of thickened, velvety, darkened skin called acanthosis nigricans
• Multiple small fluid-filled sacs in the ovaries
Although the cause of PCOS is not known, it appears that PCOS may be related to many different factors working together. These factors include insulin resistance, increased levels of hormone called androgens, and an irregular menstrual cycle.
PCOS affects all areas of the body, not just the reproductive system. It increases a woman’s risk of serious conditions that may have lifelong consequences.
Treatment:
A variety of treatments are available to address the problems of PCOS. Treatment is tailored to each woman according to symptoms, other health problems, and whether she wants to become pregnant.
Combined hormonal birth control pills can be used for long-term treatment in women with PCOS who do not wish to become pregnant. For overweight women, weight loss alone often regulates the menstrual cycle. Even a loss of 10–15 pounds can be helpful in making menstrual periods more regular. Insulin-sensitizing drugs used to treat diabetes frequently are used in the treatment of PCOS.
Endometriosis:
Endometriosis is a condition in which the type of tissue that forms the lining of the uterus (the endometrium) is found outside the uterus.
Endometriosis occurs in about one in ten women of reproductive age. It is most often diagnosed in women in their 30s and 40s.
Almost 40% of women with infertility have endometriosis. Inflammation from endometriosis may damage the sperm or egg or interfere with their movement through the fallopian tubes and uterus. In severe cases of endometriosis, the fallopian tubes may be blocked by adhesions or scar tissue.
Symptoms:
The most common symptom of endometriosis is chronic (long-term) pelvic pain, especially just before and during the menstrual period. Pain also may occur during sex. If endometriosis is present on the bowel, pain during bowel movements can occur. If it affects the bladder, you may feel pain during urination. Heavy menstrual bleeding is another symptom of endometriosis. Many women with endometriosis have no symptoms.
Diagnosis:
The only way to tell for sure that you have endometriosis is through a surgical procedure called laparoscopy. Sometimes a small amount of tissue is removed during the procedure. This is called a biopsy.
Treatment:
Treatment for endometriosis depends on the extent of the disease, your symptoms, and whether you want to have children. Endometriosis may be treated with medication, surgery, or both. When pain is the primary problem, medication usually is tried first.
Ovarian Cysts:
An ovarian cyst is a sac or pouch filled with fluid or other tissue that forms in or on an ovary. Ovarian cysts are very common. They can occur during the childbearing years or after menopause. Most ovarian cysts are benign (not cancer) and go away on their own without treatment. Rarely, a cyst may be malignant (cancer).
In most cases, cysts do not cause symptoms. Many are found during a routine pelvic exam or imaging test done for another reason. Some cysts may cause a dull or sharp ache in the abdomen and pain during certain activities. Larger cysts may cause twisting of the ovary. This twisting usually causes pain on one side that comes and goes or can start suddenly. Cysts that bleed or burst also may cause sudden, severe pain.
If your obstetrician–gynecologist (ob-gyn)or other health care professional thinks that you may have a cyst, ultrasound, blood tests and physical exams may be done.
Treatment:
There are several treatment options for cysts. Choosing an option depends on the type of cyst and other factors. Treatment options include watchful waiting and, if the cyst is large or causing symptoms, surgery.
Dr. Vaddadi practices in SIMED’s Gainesville and Lake City offices. To review any of these topics or just for general woman’s health issues, schedule an appointment with Dr. Vaddadi by calling 352-331-1000 or requesting an appointment online.
Contact our women’s health clinics:
Gainesville: 352-331-1000
You can also schedule your appointment online. Don’t wait; call or click today.