
Dr. Tina Brar of SIMEDHealth's Arthritis Center recently wrote an article for House Calls Magazine, a seasonal publication for the Alachua County Medical Society. The following article discusses advances in the treatment of psoriatic arthritis.
View the full article below:

To request an appointment with Dr. Brar, click here
Article content:
Introduction
Although psoriasis has been described since the time of Hippocrates, psoriatic
arthritis was identified as a separate disease entity in the 1960s by what is now the
American College of Rheumatology (ACR). Initially thought to be benign, it is now recognized
as a member of the spondyloarthropathies and is a debilitating, progressive illness with
a comparable impact on functional ability and quality of life as rheumatoid arthritis (RA). Early
diagnosis is imperative to prevent long-term disability and ensure optimal management of the
disease and its comorbidities.
Psoriatic arthritis (PsA) is a complex affliction with musculoskeletal involvement-
including arthritis, dactylitis, enthesitis and/or axial involvement as well as skin and nail
disease. Although the exact pathogenesis is not known, it is thought that genetic, immunologic
and environmental factors play a role. The prevalence of PsA in the United States is around
0.25%, however about 30% of patients with psoriasis also have psoriatic arthritis, affecting
men and women equally. It is therefore prudent to screen all psoriasis patients for PsA. Varying
patterns of the disease mimic different inflammatory conditions, such as gout and RA.
Approximately 15% of patients develop arthritis prior to skin involvement, making the diagnosis
difficult. Generally, laboratory tests are unhelpful as there is no specific test for PsA and
systemic inflammatory markers may be elevated in only half the cases. The genetic marker HLA-B27
is not a diagnostic test as no more than 2% of people born with this gene will eventually
develop a spondyloarthropathy. A multidisciplinary approach between dermatology and
rheumatology is helpful in analyzing many cases. Recognition of this disease process has
increased with the introduction of the classification criteria, CASPAR, as well as the development
of several screening tools that allow for timely intervention.
Treatment
Anecdotally, treatment options for PsA were limited to non-steroidal anti-inflammatory
drugs (NSAIDs) and conventional disease-modifying anti-rheumatic drugs (DMARDs).
Initially developed to treat rheumatoid arthritis, these medications have varying benefits
in treating inflammation and the vast manifestations of PsA as well. Multiple systematic reviews
have determined that the effect size of these DMARDs such as methotrexate, sulfasalazine and
leflunomide are not very high and cyclosporine is seen as toxic. Corticosteroids can be used both
locally as injections and systemically, although not supported by evidence-along with the concern
of rebound psoriasis upon withdrawal of the drug.
Spanning the past decade, the availability of targeted synthetic and biologic DMARDs
has revolutionized treatment. Given these advances, a “treat-to-target” approach towards
management has been proposed, following its favorable application in other rheumatic
conditions. The ultimate objective of therapy is to procure the lowest possible level of
disease activity in all aspects of the illness. Despite a lack of cure, there are now effective
treatments.
Tumor necrosis factor inhibitors (TNFi), which block the inflammatory mediator TNF-α, have been
around for over two decades and have established breakthrough efficacy in patients with
PsA. Five TNFi are now available, including adalimumab, etanercept, infliximab, golimumab and
certolizumab. Along with improvement in clinical signs and symptoms, these treatments
also decrease radiographic evolvement of disease. All TNF-α blockers have been studied in
randomized control trials as well as in observational studies with consistent evidence
supporting their efficacy and safety in PsA. Currently, trial data is limited in
regards to switching from one inhibitor to another, although clinically it is a successful
strategy. The choice of agent is based upon patient preference as well as regulatory and
payor requirements and/or limitations
In recent years, new biologics with alternative modes of action have also been tested
and approved in PsA. Ustekinumab is an FDA approved IL 12/23 inhibitor with evidence in
treating arthritis, skin, enthesitis and dactylitis. Guselkumab, an IL-23 blocker, is
currently FDA approved for psoriasis only and is under investigation for the management of PsA with
promising data.
Research now highlights the importance of the TL- 17 pathway and a number of therapies
targeting this pathway are being studied. FDA approved anti-IL-17 therapies include
secukinumab and ixekizumab. Currently brodalumab is FDA approved for psoriasis only,
but has shown efficacy in trials for PsA as well.
Tofacitinib is an oral inhibitor of Janus kinase that has demonstrated efficacy in the treatment of PsA in several randomized trials including patients with both an inadequate response to conventional DMARDs and TNFα(alpha) to inhibitors.
Abatacept, a selective T-cell costimulation modulator used in the treatment of
rheumatoid arthritis, has also shown benefit in patients with PsA in limited published
randomized trials and therefore became FDA-approved last year.
Apremilast, a phosphodiesterase 4 inhibitor, is a newly targeted synthetic DMARD that
induces suppression of several inflammation mediators including IL-2, IL-12, TNF-α, IFN-γ
and inducible nitric oxide synthase. Efficacy and safety in PsA has been demonstrated
through four multi-centric, randomized trials (PALACE Trials) compared to placebo in patients who
failed other biological options.
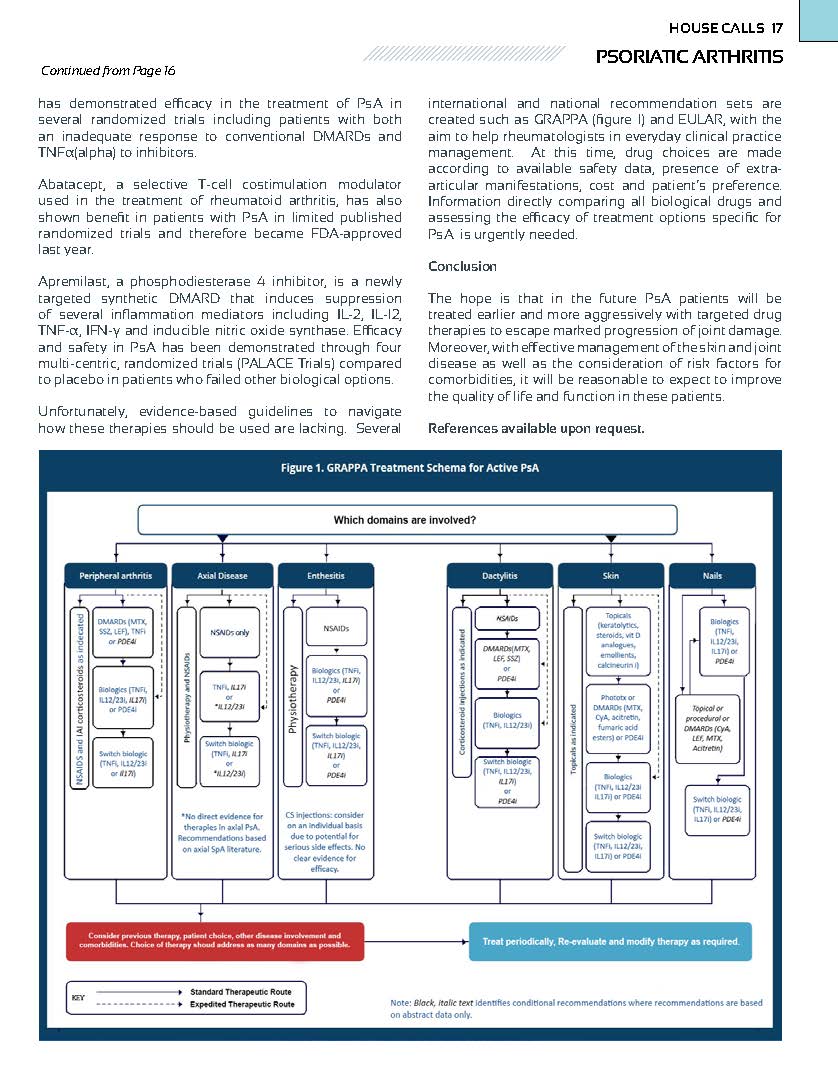
Unfortunately, evidence-based guidelines to navigate
how these therapies should be used are lacking. Several
international and national recommendation sets are created such as GRAPPA (figure 1) and
EULAR, with the aim to help rheumatologists in everyday clinical practice management. At this
time, drug choices are made according to available safety data, presence of extra-
articular manifestations, cost and patient’s preference. Information directly comparing all
biological drugs and assessing the efficacy of treatment options specific for PsA is urgently
needed.
Conclusion
The hope is that in the future PsA patients will be treated earlier and more aggressively
with targeted drug therapies to escape marked progression of joint damage. Moreover, with effective
management of the skin and joint disease as well as the consideration of risk factors for
comorbidities, it will be reasonable to expect to improve the quality of life and function in these
patients.
References available upon request.