
Sciatica – Leg Pain, Weakness, Tingling
With Dr. Juan Beyley-Pagan, a SIMEDHealth Physical Medicine and Rehabilitation physician.
1. What is sciatica?
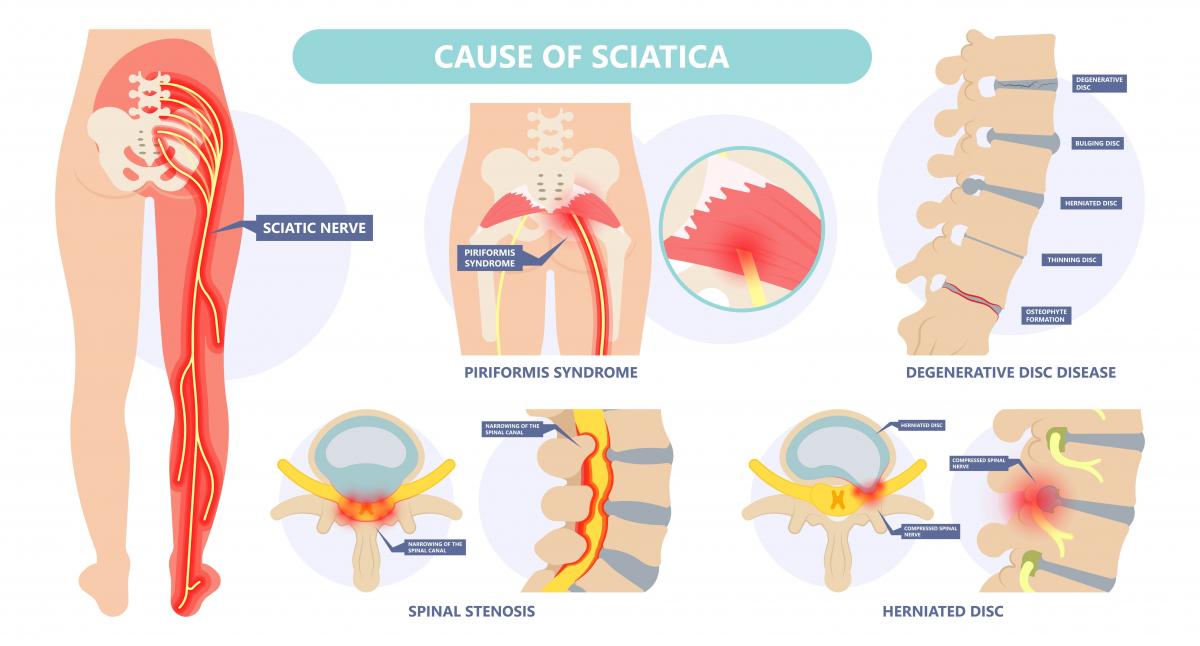
Sciatica is a broad term used for a condition causing back pain with a specific pattern of radiation down toward one lower extremity. Despite it being a well-studied syndrome, sciatica is often confused by people (including health care providers) with other sources of back pain. The word “sciatica” was adopted from Greek word “iskhiadikos” meaning “hip pain.” Today, we define sciatica as the different conditions that cause pain by affecting portions of the sciatic nerve, ranging from the nerve roots leaving the spinal canal from the 4th lumbar (L4) to the 3rd sacral (S3) spinal levels, down to where these nerves come together to create the actual sciatic nerve.
2. What are common causes of sciatic?
The most common cause of sciatica is a herniated or bulging disc somewhere in the L4 to S1 levels, which accounts for more than 90% of diagnoses. Other causes of sciatic pain may be associated with the piriformis muscle often called “piriformis syndrome.” Pelvic masses can also affect sciatic nerve but are far less common.
3. How sciatica diagnosed?
In theory, a good clinician should usually be able to diagnose sciatic pain by history and physical exam. Because >90% of sciatica comes from bulging disc, and discs are a soft tissue, to objectively identify the specific location of the condition, an MRI is the best technique for visualizing the soft tissues. If an MRI is contraindicated (due to the presence of a pacemaker, spinal cord stimulators, etc.) a CT of the lower spine could be considered. Electromyography is another technique used by physicians in the specialties of Physical Medicine & Rehabilitation, and Neurology to objectively diagnose sciatica.
4. What are treatment options for sciatica?
The treatment depends on the specific cause of the pain. For simplicity, because 90% of the sciatic pain arises from disc bulging or herniation, this discussion will focus on that source. Because nerve inflammation occurs in sciatica, anti-inflammatories are often prescribed as first line treatment. Physical therapy should be considered as soon as possible to help with pain, provide education of techniques to relieve pain, and perform some modalities (e.g.: cold or heat) to help decrease the symptoms. If conservative treatment does not provide pain relief, minimally invasive procedures such as an epidural injection could significantly relieve symptoms. Finally, if symptoms persist for several months despite conservative treatments, surgical procedures may be considered.
5. Can lifestyle changes help alleviate sciatica?
Life-style changes can definitively help sciatic pain. Sciatica is more common in individuals who are overweight, with poor back and/or pelvis posture, and/or with decreased range on motion of the back/pelvis/leg musculature. A good exercises program with core strengthening and stretching is key not only for treatment but to avoid worsening of the pain. A well-balance diet, low on grains, may help to decrease inflammation as well. Also, tobacco cessation is key for healing any musculoskeletal condition and source of pain.
Learn more about Dr. Juan Beyley-Pagan, click here.
Schedule an appointment with SIMEDHealth Rehabilitation Medicine, click here.